As we get older it is important to continue to eat well. Changes in our bodies mean that we may need less energy (calories) but we still require the same amounts of protein and important vitamins and minerals to maintain our health and well-being – we call this a nutrient dense diet. Good nutrition and regular physical activity play a protective role in a number of conditions that are more common as we get older e.g. cardiovascular disease and cognitive decline (brain function). They also help to protect oral health, bone and joint health in later life.
Also, as we get older other factors can affect our food and drink intake and make us more at risk of not getting all the nutrients we need, such as general ill health, drug interactions, being less mobile, having less income, social isolation, being depressed, suffering bereavement and poor dentition. Our general appetite may be less and we will need smaller portions of food
Malnutrition has many causes. Only when everyone responsible for nutritional support of the elderly and ill individuals (family members, doctors, nurses, dieticians, etc.) recognizes the problem in its early stages and reacts accordingly, will the affected receive adequate nutritional support. It is essential that all professional groups work closely together to solve the problem of malnutrition. We must realize that despite the well-designed nutritional support we are not reaching our goal.
Key dietary problems in older people:
- . Protein- energy malnutrition (herein referred to as “malnutrition”) in older people is characterized by involuntary weight loss and muscle wasting secondary to inadequate dietary.
• Overweight and obesity are prevalent in well older people but this decreases in further old age.
• Low intakes of protein, vitamin D, and iron which impact on overall health.
• Constipation is common as food intake reduces, activity decreased and can be made worse by dehydration.
. Oral health and dietary intake are also closely linked – having poor oral health, tooth decay, and gum disease can reduce food intake and enjoyment of food and have a big impact on quality of life.
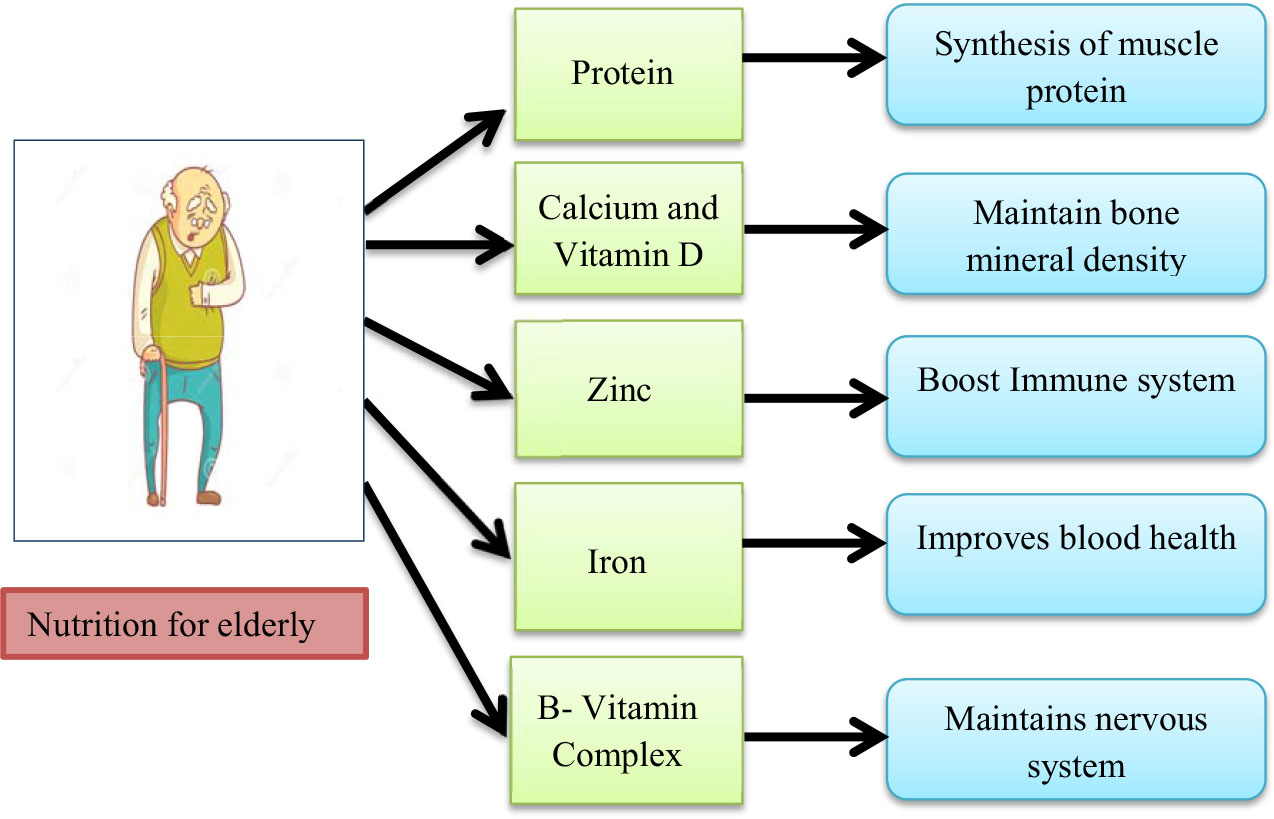
Important nutrients
*Energy although energy requirements may be less, the quality of the diet needs to be the same. However, some elderly may have increased energy requirements, for example if they have chronic obstructive pulmonary disease (COPD) or Parkinson’s disease. with dementia may have lower energy requirements if less mobile with low motivation, or they may be increased in the case of hyperactivity, restlessness and being more active.
*Protein intakes are important to preserve muscle mass and help to prevent sarcopenia as well as having a crucial role in wound healing and maintenance of pressure areas.
*Dietary Fibre is important to help prevent constipation, which is more common in older people, and is a valuable source of nutrients.
*Vitamin D There are specific recommendations for vitamin D for older people. Vitamin D is synthesized in the skin via the action of sunlight. It is essential for bone health and believed to improve muscle strength. Older people typically go out doors less than younger age groups and their skin is less efficient at producing vitamin D from sunlight.
*Iron Poor food intakes of iron can lead to iron deficiencies in older people, causing tiredness and dizziness and can result in anemia.
References:
1. Nutrition Screening Survey in the UK and the republic of Ireland (BAPEN, 2011) Hospitals, Care Homes and Mental Health Units https://www.bapen.org.uk/pdfs/nsw/nsw_report2008-09.pdf

